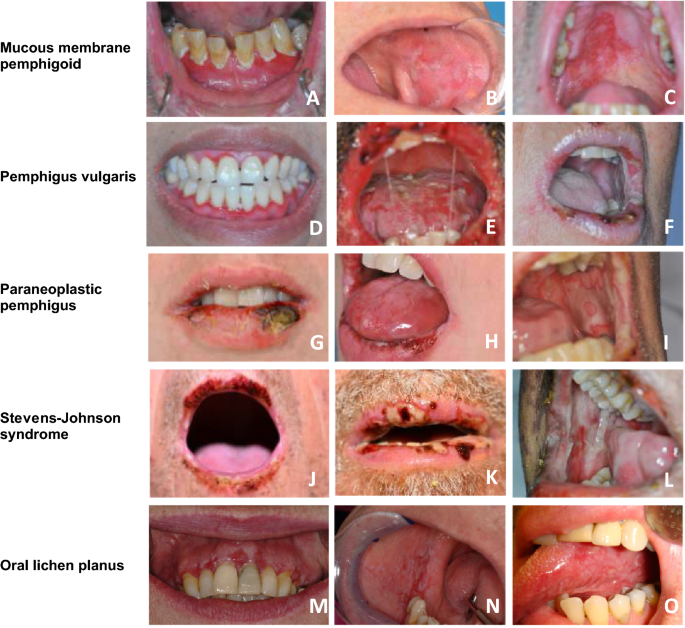
Autoimmune Diseases With Oral Manifestations
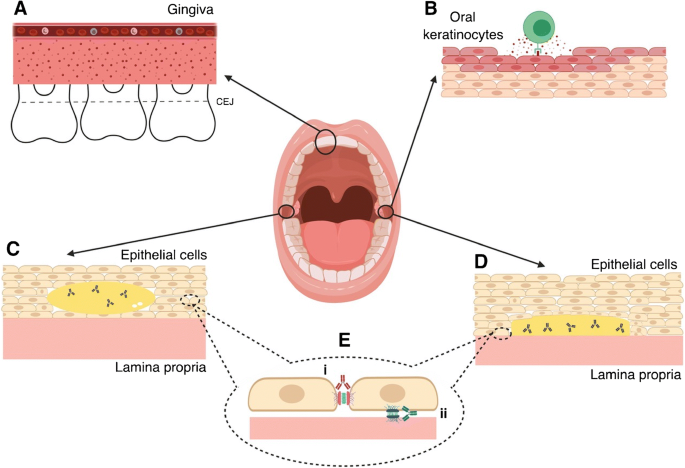
Autoimmune diseases can present with oral manifestations, affecting the mucosa, salivary glands, and periodontal tissues. These conditions may lead to xerostomia, oral ulcers, and gingivitis, among other symptoms.
Understanding the link between autoimmune diseases and oral health is crucial for proper diagnosis and management. Autoimmune diseases, such as lupus, Sjögren’s syndrome, and pemphigus vulgaris, can impact oral health in various ways. Recognizing these manifestations early on can aid in timely intervention and improved quality of life for patients.
We will explore the relationship between autoimmune diseases and oral health, highlighting common oral symptoms associated with these conditions and the importance of interdisciplinary care in managing these complex health issues.

Credit: www.sciencedirect.com
Common Autoimmune Diseases
Rheumatoid Arthritis
Rheumatoid Arthritis is an autoimmune condition that primarily affects the joints, causing pain and swelling. It can also lead to oral manifestations such as gum inflammation and periodontal disease. In some cases, patients may experience dry mouth, making them more susceptible to dental cavities and oral infections.
Systemic Lupus Erythematosus
Systemic Lupus Erythematosus, or lupus, is a chronic autoimmune disease that can impact various parts of the body, including the mouth. Oral symptoms may include mouth sores, oral ulcers, and a condition known as lupus stomatitis, which causes redness and lesions on the oral mucosa. Patients with lupus may also experience dry mouth and an increased risk of dental decay.
Sjögren’s Syndrome
Sjögren’s Syndrome is characterized by dryness in the mouth and eyes due to the immune system attacking the body’s moisture-producing glands. This can result in a range of oral manifestations, including dry mouth, difficulty swallowing, and an increased risk of dental caries. Additionally, individuals with Sjögren’s Syndrome may develop oral yeast infections and experience a reduced sense of taste.
Oral Manifestations
Oral Manifestations:
Mucosal Ulcers
Mucosal ulcers are common in autoimmune diseases, causing painful sores in the mouth.
Xerostomia (dry Mouth)
Xerostomia, or dry mouth, is a symptom where there is a decrease in saliva production.
Oral Lichen Planus
Oral lichen planus is a chronic inflammatory condition that affects the mucous membranes in the mouth.
Diagnostic Challenges
Autoimmune diseases can have oral manifestations that can cause significant diagnostic challenges for healthcare professionals. The oral symptoms can often be the first signs of an underlying autoimmune disease, which makes early detection and diagnosis essential for effective treatment. However, the overlap of oral pathologies and the difficulty in distinguishing them from autoimmune oral manifestations can pose a challenge.
Overlap With Oral Pathologies
Oral pathologies such as infections, trauma, and neoplasms can present symptoms similar to those of autoimmune diseases. For instance, oral lichen planus, a common autoimmune disorder affecting the mucous membranes of the mouth, shares clinical features with other non-autoimmune oral diseases such as lichenoid drug reactions and lichenoid contact stomatitis. The similarities in clinical presentation can make it challenging for healthcare professionals to distinguish autoimmune oral manifestations from non-autoimmune pathologies.
Importance Of Multidisciplinary Approach
Given the diagnostic challenges posed by autoimmune diseases with oral manifestations, a multidisciplinary approach is critical to achieving an accurate diagnosis. A team of healthcare professionals, including rheumatologists, dermatologists, gastroenterologists, and dentists, can work together to evaluate the patient’s symptoms and medical history and arrive at a definitive diagnosis. Collaboration between these specialists can help identify the underlying autoimmune disease and provide appropriate treatment.
Furthermore, comprehensive clinical assessment and laboratory testing are essential for accurate diagnosis and effective treatment of autoimmune diseases with oral manifestations. A biopsy of the affected tissue can help in the diagnosis of autoimmune oral disorders. The healthcare professional must take into account the patient’s symptoms, medical history, and laboratory test results to arrive at the correct diagnosis.
In conclusion, autoimmune diseases with oral manifestations present a diagnostic challenge for healthcare professionals. Given the overlap with non-autoimmune oral pathologies, a multidisciplinary approach involving specialists from various medical fields is essential to achieve an accurate diagnosis. Early detection and diagnosis of autoimmune diseases with oral manifestations can help in effective treatment and management of the patient’s condition.
Credit: link.springer.com
Treatment Approaches
When it comes to the treatment of autoimmune diseases with oral manifestations, it is essential to address both the systemic and oral symptoms. The management of these conditions requires a multidisciplinary approach that focuses on controlling the underlying autoimmune response while also alleviating the specific oral manifestations.
Managing Oral Symptoms
The management of oral symptoms in autoimmune diseases involves a combination of pharmacological and non-pharmacological interventions. Dentists and oral health professionals play a crucial role in providing symptomatic relief and preventing further oral complications. This may include the use of topical corticosteroids, immune-modulating agents, and pain management strategies to address oral lesions and discomfort.
Collaborative Care With Rheumatologists/dermatologists
Collaborative care with rheumatologists and dermatologists is essential for managing autoimmune diseases with oral manifestations. This interdisciplinary approach allows for a comprehensive evaluation of the patient’s condition, leading to tailored treatment plans that address both the systemic and oral symptoms. Close communication and shared decision-making among healthcare providers ensure that the patient receives holistic care that considers the impact of systemic treatments on oral health and vice versa.
Impact On Quality Of Life
Autoimmune diseases with oral manifestations can significantly impact the quality of life, causing pain and discomfort in everyday activities. Managing symptoms through proper treatment and care is crucial for improving overall well-being and reducing the burden of these conditions.
Impact on Quality of Life Living with autoimmune diseases that exhibit oral manifestations can significantly impact an individual’s quality of life. The pain and discomfort experienced, as well as the psychosocial effects, can have a profound influence on daily activities and overall well-being. Pain and Discomfort The oral manifestations of autoimmune diseases often lead to persistent pain and discomfort. This can affect essential functions such as eating, speaking, and even smiling. As a result, individuals may experience difficulty in performing routine tasks, leading to a decreased quality of life. The discomfort caused by oral manifestations can also result in sleep disturbances and overall fatigue, further impacting the individual’s ability to engage in daily activities. Additionally, the pain may necessitate frequent visits to healthcare providers, leading to disruptions in work or personal schedules. Psychosocial Effects The visible nature of oral manifestations can lead to self-consciousness and social anxiety. Individuals may feel hesitant to engage in social interactions, affecting their relationships and overall mental well-being. Furthermore, the psychosocial effects of autoimmune diseases with oral manifestations can lead to feelings of isolation and depression. Coping with the visible symptoms and managing the associated discomfort can be emotionally taxing, impacting the individual’s overall quality of life. In conclusion, the impact of autoimmune diseases with oral manifestations on an individual’s quality of life cannot be understated. The combination of pain, discomfort, and psychosocial effects can significantly hinder daily activities and overall well-being. Therefore, it is crucial to address these challenges effectively to improve the quality of life for individuals living with these conditions.
Credit: www.sciencedirect.com
Preventive Oral Care
Preventive oral care is crucial for individuals with autoimmune diseases as they are more prone to oral manifestations such as dry mouth, oral ulcers, and gum disease. Ignoring oral health can lead to severe consequences, including tooth loss and infections. Therefore, it is essential to follow proper oral hygiene practices and schedule regular dental check-ups.
Importance Of Regular Dental Check-ups
Regular dental check-ups help detect any oral issues at an early stage and prevent them from worsening. Individuals with autoimmune diseases should visit their dentist twice a year to monitor their oral health. During a dental check-up, the dentist will check for signs of gum disease, cavities, and oral cancer. They will also evaluate the impact of medication on oral health and provide recommendations accordingly.
Oral Hygiene Recommendations
Individuals with autoimmune diseases should follow these oral hygiene recommendations to maintain good oral health:
- Brush teeth twice a day with a soft-bristled brush and fluoride toothpaste.
- Floss daily to remove plaque and food particles between teeth.
- Use an antiseptic mouthwash to reduce the risk of infections.
- Avoid smoking and tobacco products as they increase the risk of oral cancer and gum disease.
- Stay hydrated to prevent dry mouth, a common side effect of autoimmune disease medication.
- Consume a balanced diet rich in vitamins and minerals to strengthen teeth and gums.
By following these oral hygiene recommendations and scheduling regular dental check-ups, individuals with autoimmune diseases can maintain good oral health and prevent oral manifestations from worsening.
Conclusion
Understanding oral manifestations of autoimmune diseases is crucial for early detection and treatment. Maintaining good oral hygiene and regular dental check-ups play a significant role in managing these conditions. By staying informed and proactive, individuals can better manage their overall health and well-being.